VITA ENAMIC absorbs masticatory forces: New findings from an in vitro test
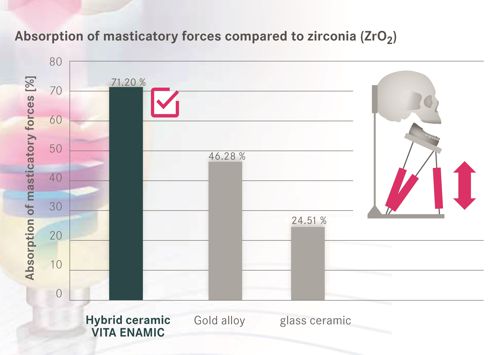
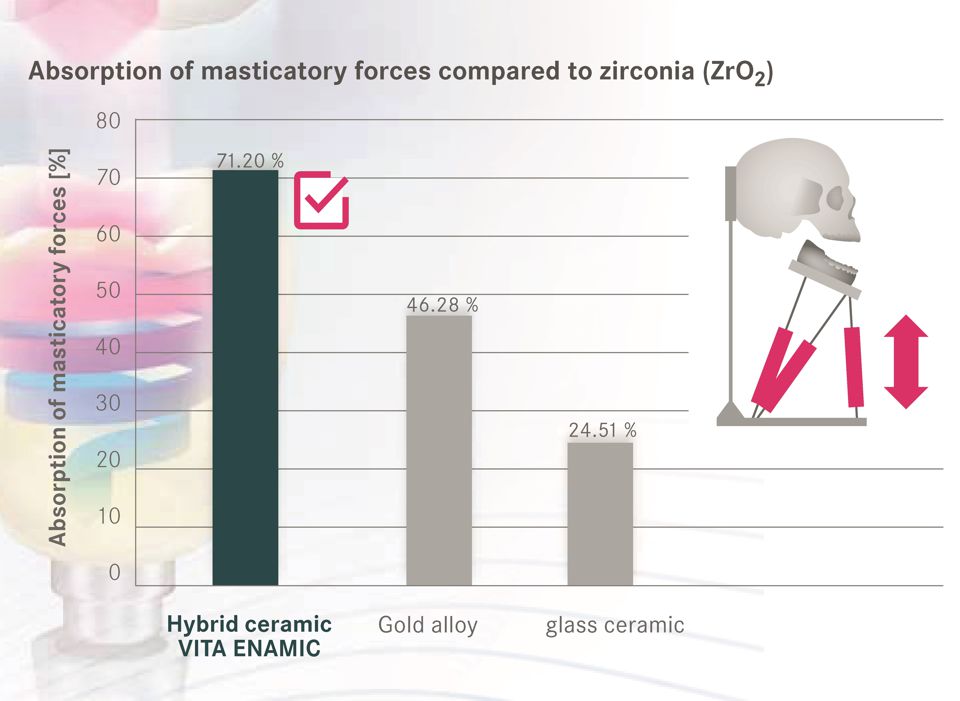
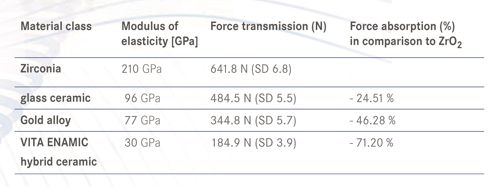
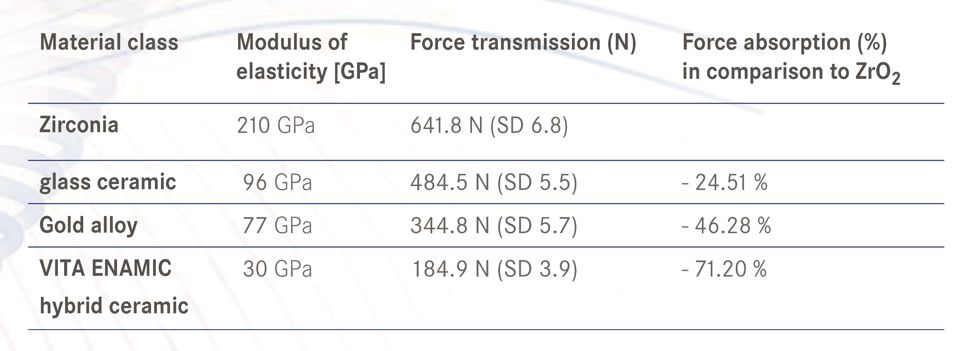
Study results from a chewing simulator regarding force transmission on a simulated peri-implant bone show that crowns made of a relatively elastic material such as the hybrid ceramic VITA ENAMIC can reduce or absorb about 70 percent of the force compared to crowns made of the comparably rigid zirconia. Dr. Maria Menini reports on her findings in a test series in the following interview.
DV: Dr. Menini, what results have you determined for hybrid ceramics in comparison to zirconia and glass ceramics with regard to the ability to absorb masticatory forces?
Dr. Maria Menini: In the investigations that our research team conducted under the leadership of Prof. Dr. Paolo Pera, the restoration material used had a significant impact on the transmission of masticatory forces to the simulated peri-implant bone. By using elastic materials, the measured load transmission could be reduced. The hybrid ceramics in particular demonstrated a shock absorbing behavior in comparison to zirconia and glass ceramics. This reduced the forces transmitted to the bone-implant interface.
DV: Why do relatively elastic materials such as VITA ENAMIC have a better ability to absorb masticatory forces than traditional glass or oxide ceramics, for instance?
Dr. Maria Menini: Elastic materials absorb masticatory forces by deforming under a load – similar to a mattress that you would jump on. In contrast, more rigid materials such as zirconia do not offer this property, so that applied forces are transmitted directly to the underlying structures (e.g., implant and bone). Hooke's law applies here: The more rigid the material (i.e., the higher the modulus of elasticity), the lower the deformation under load and the greater the force transmission and vice versa.
DV: What are the risks that may result with an implant-supported restoration from a relatively direct and rigid connection between bone and implant?
Dr. Maria Menini: In contrast to natural teeth, osseointegrated implants are rigidly anchored in the bone. This leads to a direct transmission of force to the peri-implant bone under a load. With physiological loading of the osseointegrated implant, the bone substance does actually adjust (i.e. bone turnover processes), but an excessive overload can lead to bone fractures, bone resorption and technical complications. As a result, it appears to be important to ensure a controlled force transmission on the bone-implant interface.
DV: Can elastic restoration materials possibly minimize these risks in implant restorations due to their ability to absorb masticatory forces?
Dr. Maria Menini: Results from in-vitro studies indicate that this is possible, but clinical data is not yet available. According to our tests in the chewing simulator, the use of hybrid ceramics, composite and acrylic resins reduces the forces transmitted on the bone-implant interface approximately 70 to 95 percent in comparison to zirconia. These findings should be taken into consideration when selecting the restoration material, especially in cases where the load must be minimized (e.g. in the context of immediate restoration).
DV: For what other clinical indications may the use of restoration materials with "forceabsorbing" properties be especially sensible, and why?
Dr. Maria Menini: It can be prudent to use elastic materials if clinicians want to reduce the occlusal load. This applies for restorations on implants and on natural tooth substance, for example in patients with parafunctions. What biomechanical effects the use of relatively more rigid restoration materials such as ceramics have on the masticatory system has not been investigated up to now. With materials containing polymer and showing tooth-like properties, however, possible negative effects could be prevented.
Report 09/15